Click through to the October 2019 digital magazine for the complete article.
Sensitive skin is a condition of cutaneous hyperreactivity that can result in exaggerated reactions to physical, chemical, hormonal and/or psychological factors. It affects more than 50% of the world's population; in fact, one epidemiological study reported a prevalence of 38.4% in the whole of Europe alone.1
Two primary processes contribute significantly to hypersensitized skin: an acceleration of nerve responses, leading to neurogenic inflammation; and an increase in stratum corneum permeability due to an impaired barrier.2 The Transient Receptors Potential Vanilloid (TRPV) channels play a central role in both of these processes. These cationic receptor channels mediate the influx of monovalent and/or divalent cations into the cells in response to a variety of chemical or physical stimuli.
In the skin, TRPV channels are expressed in most cell types, including keratinocytes, sensory neurons, melanocytes and immune cells. Among the TRPV channels, TRPV1 is the most extensively characterized as it is involved in neurogenic inflammation and hypersensitive skin conditions.3 An activation of TRPV1 by either chemical or mechanical stimuli results in a local, intracutaneous release of a plethora of neuropeptides, such as substance P and tachykinins, as well as the Calcitonin Gene-Related Peptide (CGRP).4
The released peptides activate multiple types of skin cells including keratinocytes, mast cells, fibroblasts, endothelial cells and sebocytes, and induce the production of proinflammatory and vasoactive substances such as proinflammatory cytokines. Moreover, TRPV1 negatively affects the skin barrier by delaying its recovery after injury.5
In contrast, two other receptor family members, TRPV3 and TRPV4, positively influence skin barrier formation. TRPV3 activation has been shown to control keratinocyte migration and wound healing,6 and to stimulate two important skin growth factors: TGF-α and EGF.7 Moreover, the pharmacological activation of TRPV4 appears to accelerate barrier regeneration in mice8 while TRPV4-deficient mice show a pathological impairment of the epidermal barrier.9
The present authors sought ingredients to fight sensitive skin conditions specifically by acting on TRPV channels. As shown here, a water-soluble extract derived from aubergine (Solanum melongena) cell suspension cultures was identified as capable of inhibiting the expression of the negative regulator TRPV1 while enhancing those of the positive regulators TRPV3 and TRPV4. These in vitro results were supported by clinical tests in human volunteers, also shown here, which indicated the extract alleviated cutaneous hyperreactivity, as shown by stinging test, and improved the skin barrier function by reducing water loss, as shown by TEWL measure. The aubergine extract is therefore presented as a new potential active for skin care products specifically addressing sensitive skin.
Materials: Plant Extract and Cell Cultures
S. melongena (aubergine) cells were grown as suspension cultures in Gamborg B5 mediuma supplemented with: 500 mg/L myo-inositol, 30 g/L sucrose, 1 mg/L 2,4-dichlorophenoxyacetic acid (2,4-D), 0.1 mg/L kinetin and 1 mg/L adenine. The cultures were maintained at 27°C in the dark under constant orbital stirring (110 rpm). After the cells reached a density of approximately 0.3 kg/ L, they were collected and lysed in a phosphate buffer—i.e., 136 mM NaCl, 2.7 mM KCl, 12 mM NaH2PO4 and 1.76 mM KH2PO4 at pH 7.4—to prepare a water-soluble (hydrosoluble) extract, referred to here as S. melongena hydrosoluble extract (SmHE). The resulting solution was then collected and lyophilized in order to obtain a fine powder that was easy to dissolve in water or cell culture media for testing.
The active ingredient for skin care formulas is prepared by dissolving the extract in glycerol at 0.4% and using the solution at 0.5% in the final bulk; a formula containing S. melongena cell culture extract, and used in the described clinical studies, is provided in Formula 1.
The skin cell cultures used in the assays were skin keratinocytes (HaCat cell line) and macrophages (RAW 264.7 cells).
In vitro Methods
Cell vitality (MTT assay): To determine any potential cytotoxicity of the extract, 1 x 104 keratinocytes were seeded in 96-well plates, grown for 8 hr at 37°C and 5% CO2 and treated for 48 hr with different concentrations of it. After treatment, keratinocytes were washed with PBS and incubated with 100 μL/well of “reaction buffer” containing: 10 mM Hepes, 1.3 mM CaCl2, 1 mM MgSO4, 5 mM glucose and 0.5 mg/mL of the colorimetric substrate MTT [3-(4,5-dimethylthiazolyl)-2,5-diphenyltetrazolium bromide] in PBS buffer at pH 7.4. This protocol followed that described by Mosmann et al.10 After 3 hr, the cells were solubilized by the addition of 100 μL of solution (10% octylphenol ethoxylateb; 0.1 N HCl in isopropanol), and the plate incubated for 4 hr at room temperature. The number of healthy cells was directly proportional to the level of the formazan product created. The developed color was then quantified at 595 nm by a multiple plate readerc.
Proinflammatory cytokines and TRPV1 gene expression: For gene expression analysis of the inflammatory cytokines IL-6, IL-8 and TNF-α, and of TRPV1, keratinocytes were incubated with SmHE for 16 hr and treated with LPS (a bacterial lipopolysaccharide)d at 5 μg/mL for 3 hr. Then, total RNA was collected by using an RNA purification kit according to the manufacturer’sd instructions. The results were compared to those obtained by the synthetic drug T0901317, used as the positive control.
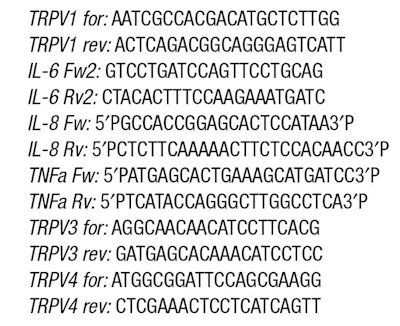
TRPV3 and TRPV4 gene expression: For gene expression analysis of TRPV3 and TRPV4, keratinocytes were incubated for three days with the test compounds to allow the cells to differentiate, then processed for total RNA extraction. Reverse transcription polymerase chain reaction (RT-PCR) was performed using gene-specific primers and an oligonucleotide internal standard kite. The PCR products obtained were visualized and quantified by an imaging systemf. The amplification band corresponding to the analyzed gene was normalized to the amplification band corresponding to the 18S. The values obtained were finally converted into percentage values by considering as 100% the measure of the samples of LPS-stimulated cells. The specific primers used are listed in the sidebar Gene-specific Primers for Cytokine and TRPV Analysis. . .
Continue reading in the October 2019 digital magazine...