Benzoyl peroxide (BPO) has been used as an anti-acne treatment for several decades. Its unique activity is based on the ability to not only reduce Propionibacterium acnes, but also to decrease inflammatory lesions. As is well-known, P. acnes is the bacteria responsible for acne breakouts and it cannot live in an aerobic (i.e., oxygen-rich) environment. Benzoyl peroxide works by introducing oxygen into the pore, thereby killing the bacteria and, in turn, reducing the number of breakouts on the skin. And since BPO acts as a toxin on P. acnes rather than an antibiotic, resistance to BPO does not occur and has not been reported. Another factor that makes benzoyl peroxide so effective is its ability to help rid the follicle of excess dead skin cells since clearing the pore of cellular debris lessens the chances of pore blockages, or comedones. In this way, benzoyl peroxide helps to prevent breakouts before they start.
Regarding its regulation, the final Federal Register monograph of the US Food and Drug Administration (FDA), published on March 4, 2010, classified BPO as a safe and effective over-the-counter (OTC) topical acne drug product. This monograph went into effect on March 4, 2011, having taken more than 20 years to establish due to safety precautions. The monograph permits the use of BPO at levels between 2.5% and 10.0%; common commercial drug products, such as wash-off or leave-on gels or creams, typically use concentrations of 2.5% and 5.0%, up to 10.0%.
BPO commonly causes initial dryness and sometimes irritation, although skin tolerance usually occurs after a week or so.2, 8 However, a small percentage of individuals are much more sensitive to it and can suffer burning, itching, peeling and possibly swelling. It therefore is sensible to apply the lowest concentration to build up skin’s tolerance, as appropriate. Once tolerance is achieved, increasing the quantity or concentration a second time and gaining tolerance at a higher level usually gives better subsequent acne clearance.2, 9
Irritation and Efficacy
In relation to this increase in concentration to build skin tolerance, an unanswered question arose from a clinical test on 153 patients by Mills et al. in 1986.10 During this test, it was found that 5% and 10% concentrations were not significantly more effective than 2.5%, although 2.5% was usually better tolerated. In addition, the 2.5% BPO formulation was more effective than its vehicle and equivalent to the 5% and 10% concentrations in reducing the number of inflammatory lesions, i.e., papules and pustules. Desquamation, erythema and symptoms of burning with the 2.5% gel were also less frequent than with the 10% preparation but equivalent to the 5% gel. The 2.5% formulation also significantly reduced P. acnes and the percentage of free fatty acids in the surface lipids after two weeks of topical application. The review article of recent advancements of BPO anti-acne formulas by Fakhour et al. also concluded that BPO in concentrations of 2.5%, 5% and 10% were equally effective at treating inflammatory acne. However, higher concentrations were associated with more adverse effects. 2
BPO Structure, Solubility
To understand these clinical results, it helps to consider the properties of BPO. The structure of BPO, shown in Figure 1, is nearly symmetrical and non-polar, and is poorly soluble in water. Owing to this molecular structure, it is almost insoluble in common personal care solvents such as ethanol, glycerin, propylene glycol or butylene glycol. The solubility of BPO in water is only 9.1 ppm at 25°C (9.1 mg/L);11 therefore, in most acne products, BPO is suspended as a fine powder consisting of various sizes of clumps of BPO molecules that are deposited on the surface of the skin. These clumps exhibit limited penetration into the skin and limited mobility on the skin since powder does not move freely. This lack of mobility results in dose-dependent skin irritation and dose-independent efficacy.12, 14
For years, improving the solubility of BPO has been explored to increase its anti-acne efficacy while decreasing its irritation. In 2002, Popp and Stiefel disclosed a method using dimethyl isosorbide (DMI) to dissolve BPO and applied it in two prescription-only product lines—each including a creamy wash, cleansing cream or lotion, and gel—containing BPO at 4% and 8%, respectivelya.13, 14 The technique, called hydrophase, involves: 1) heating water to between 60°C and 70°C; 2) adding a detergent base to the water and mixing the solution; 3) cooling the solution and adding an alpha hydroxy acid, an isosorbide and sodium pyrollidone carboxylate; 4) cooling the solution to between 25°C and 35°C, then adding benzoyl peroxide and a preservative to the solution; 5) mixing and milling the product until smooth; and 6) adjusting the pH of the product to 3–5 with a base.
In relation, six-week clinical studies of some 567 patients in India were conducted to assess the efficacy and irritation potential of the 4% BPO cream in a hydrophase base compared with the same percentage of powder suspension BPO cream for the treatment of Acne vulgaris.12 The patients were evaluated at baseline and at 1, 2, 4 and 6 weeks. Patients also rated observed improvements and any adverse effects. Dermatologist assessments showed that by the end of week six, 85.6% of the individuals experienced good to very good treatment effects. Side effects profiling revealed that 53.8% of patients did not show any irritation, whereas only 11.6% showed moderate to severe irritation. In addition, 53.8% of patients did not report any irritation, 41.4% reported some irritation, and only 4.8% reported troublesome irritation.
A “satisfactory” response from patients was reported as early as two weeks, and most patients reported a “very satisfactory” response after six weeks and were willing to continue the treatment. This supports the theory that the hydrophase formulation in products helped to enhance efficacy and decrease the irritation associated with the use of BPO. Similar results on the same test product in both leave-on and wash-off forms were observed by Weinberg,1 including the reduction of P. acnes and decrease in both inflammatory lesions/irritation and emergence of antibiotic-resistant P. acnes strains, in comparison with other BPO preparations. As previously mentioned, since the effect of BPO on P. acnes is a direct toxic effect rather than antibiotic in nature, resistance does not occur and has never been reported. The authors therefore conclude that the low irritancy of this product is related to the unique delivery vehicle containing DMI, which dissolves BPO crystals. Another US patent explored the use of a different solvent system to solubilize BPO14 containing a member of the group consisting of aryl esters of both benzyl alcohol and benzoic acid to provide a stable peroxide solution. This system, also including benzyl benzoate and DMI, was developed commercially in a product lineb including a three-step system of a cleanser and pore therapy toner containing 2.0% salicylic acid, and an anhydrous serum gel with 5.0% BPO.
The marketer conducted various clinical studies, the results of which were presented and/or published at various conferences and in several journals.15–22 Using scanning electron microscopy, Spellman et al. showed that the solubilized 5.0% BPO serum did not leave visible BPO crystals on skin. In comparison, the traditional BPO products showed crystalline powder, clearly deposited on the skin.16 Overall, the clinical studies concluded that solubilized BPO products increased the follicular penetration of BPO, improved P. acnes kill rates and clinical efficacy, and improved tolerability.15 The solubilized BPO acne treatment systems demonstrated enhanced penetration of BPO into the sebaceous follicles and, as part of a specific regimen, appears to offer advantages over the traditional combination of BPO and clindamycin with respect to efficacy and comfort to skin. 17, 18
BPO Solubility: Physical Principles
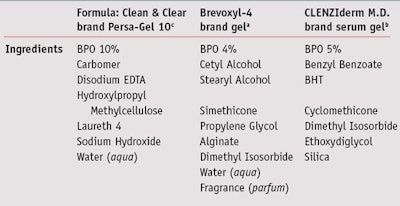
A comparison of a traditional BPO crystalline powder suspensionc and two solublized BPO formulations is shown in Table 1. The ingredients listed were taken from commercial product labels. The traditional formula uses neutralized carbomer and hydroxypropyl methylcellulose to suspend a 10% BPO formula.
The reason this formula was chosen is that it represents the conventional approach to suspending powder by use of polymers such as carbomers and hydroxypropyl. Polymers are critical to stabilizing powder BPO in the formulas for longer shelf life. In general, this suspension formula poses some whitening on the skin from crystalline BPO and needs several rubs to disperse it.
The other two formulas included solubilized BPO; they did not impart whitening on the skin and instead gave more emollient and moisturizing effects. The solvent dimethyl isosorbide was used in the productsa with several other common skin sensory ingredients such as cetyl and stearyl alcohol and simethicone. It is interesting to note that alpha hydroxy acid and sodium pyrollidone carboxylate were not used in the formulas, which are part of hydrophase claim in patent.12 Both dimethyl isosorbide and benzyl benzoate solvents were used in the solubilized gel creamb; this anhydrous formula takes a different approach at stabilizing solubilized BPO in that the continuing phase is thickened by silicac.
Discussion
It has taken several decades for the industry to realize that improving the solubility of BPO can improve its efficacy and decrease irritation. However, these challenges can be rationalized in that BPO is a strong oxidizing agent, and solubilized BPO would thus be more reactive than its crystalline powder. It is also challenging to make products that are stable for commercial use and to find adequate solvents since BPO is not soluble in most. Reviewing the structures of benzyl benzoate and dimethyl isosorbide—the only solvents known to successfully solubilize BPO—they are similar to BPO (see Figure 2), which follows the rule of “like dissolves like.” These two solvents are less common and therefore more expensive, in addition to being patent-protected. Such technologies are therefore only used in prescription and high-end products. The testing of more solvents based on the “like dissolves like” rule could assist the industry in discovering other effective, lower cost solvents for BPO in the future.
References
Send e-mail to [email protected].
1. JM Weinberg, The utility of benzoyl peroxide in hydrophase base (Brevoxyl) in the treatment of Acne vulgaris, J Drugs Dermatol 5(4) 344–349 (2006)
2. T Fakhouri, BA Yentzer and SR Feldman, Advancement in benzoyl peroxide-based acne treatment: Methods to increase both efficacy and tolerability, J Drugs Dermatol 8(7) 657–661 (2009)
3. E Eady, R Bojar, C Jones, J Cove, K Holland and W Cunliffe, The effects of acne treatment with a combination of benzoyl peroxide and erythromnycin on skin carriage of erythromycin resistant propionibacteria, Br J Dermatol, 134 (1996)
4. GA Taylor and AR Shalita, Benzoyl peroxide-based combination therapies for acne vulgaris: A comparative review, Am J Clin Dermatol 5 261–265 (2004)
5. US Food and Drug Administration Final Monograph, Federal Register 75(42) 9767–9777 (Mar 4, 2010)
6. US Food and Drug Administration Tentative Final Monograph, FR Citation: 50 FR2172 (Jan 15, 1985)
7. US Food and Drug Administration Proposed Rule, Reclassifies benzoyl peroxide from GRASE to Category III, FR Citation: 56FR37622, available at www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/Development Resources/Over-the-CounterOTCDrugs/Status ofOTCRulemakings/UCM181724.pdf Aug 7, 1991 (Accessed May 16, 2011)
8. M Jelvahgari, MR Siahi-Shadbad, S Azarmi, GP Martin and A Nokhodchi, The microsponge delivery system of benzoyl peroxide: Preparation, characterization and release studies, Int J Pharm 308 124–132 (2006)
9. WJ Cunliffe, KT Holland, R Bojar and SF Levy, A randomized, double-blind comparison of a clindamycin phosphate/benzoyl peroxide gel formulation and a matching clindamycin gel with respect to microbiologic activity and clinical efficacy in the topical treatment of acne vulgaris, Clin Ther 24 1117–1133 (2002)
10. OH Mills Jr, AM Kligman, P Pochi and H Comite, Comparing 2.5%, 5% and 10% benzoyl peroxide on inflammatory acne vulgaris, Int J Dermatol 25(10) 664–67 (1986)
11. Benzoyl peroxide, 2002United National Environment Program document, available at www.chem.unep.ch/irptc/sids/oecdsids/ BENZOYLPER.pdf 5 (Accessed May 16, 2011)
12. US Patent 6,433,024, Topical anti-acne composition, assigned to KF Popp and BD Stiefel (May 8, 2002)
13. SN Sawleshwarkar, V Salgaonkar and CM Oberai, Multicenter study to evaluate efficacy and irritation potential of benzoyl peroxide 4% cream in hydrophase base (Brevoxyl) in Acne vulgaris, Indian J Dermatol Venereol Leprol 69(1) 19–22 (2003)
14. US Patent 7,390,431, Stable organic peroxide compositions, JR Faryniarz and JE Ramirez, assigned to JR Chem, LLC (Mar 10, 2006)
15. J Leyden, New Developments in topical antimicrobial therapy for acne, J Drugs in Dermatol 7(2 suppl) 8–11 (2008)
16. MC Spellman and J Ramirez, a Comparison of patterns of deposition of two formulations of benzoyl peroxide on the skin and in the Follicular ostia as visualized by scanning electron microscopy, poster presentation, Annual American Academy of Dermatology meeting (2007)
17. LF Eichenfield et al, A Three-step acne system containing solubilized benzoyl peroxide versus benzoyl peroxide/Clindamycin in pediatric patients with acne, J Clin Aesthetic Dermatol 2(11) 21–26 (2009)
18. L Kircik et al, The pharmacologic science of a novel benzoyl peroxide formulation and the implications for clinical effects, poster presentation, 25th Anniversary Fall Clinical Dermatology Conference (Oct 6–9, 2006)
19. L Kircik et al, Comparing a novel solubilized benzoyl peroxide gel with benzoyl peroxide/Clindamycin: Final data from a multicenter, investigator-blind, randomized study, J Drugs Dermatol 8(9) 812–818 (2009)
20. D Thiboutot et al, A 3-step acne system containing solubilized benzoyl peroxide versus Clindamycin-benzoyl peroxide, Cutis 84(1) 48–55 (2009)
21. JQ Del Rosso, Evaluation of a solubilized benzoyl peroxide gel: A pooled analysis from 3 randomized investigator-blinded trials, Cos Derm 21(10) 201–206 (2008)
22. E Tanghetti, L Kircik, D Wilson and S Dhawan, Solubilized benzoyl peroxide versus benzoyl peroxide/Clindamycin in the treatment of moderate acne, J Drugs Dermatol 7(6) 534–538 (2008)