Hair color is an important part of one’s identity. However, hair dye allergic contact dermatitis remains a problem for many; its prevalence among patients is reported as 4.3% in Asia, 4% in Europe and 6.2% in North America.1 P-Phenylenediamine (PPD) is a common ingredient and sensitizer in oxidative hair dye products that can lead to contact allergy dermatitis. While this is thought to be the most common sensitizer, there are more than 100 permitted chemicals in hair dye, and many have been identified as possible sensitizers.2 As a result, it is difficult prior to patch testing to determine which ingredient is causing the reaction.
Here, the authors describe the typical presentation and symptoms resulting from hair dye allergic contact dermatitis. Common chemical sensitizers in hair dye and the utility of patch testing are detailed, and interventions and prevention principles for those who wish to continue dyeing their hair are outlined—with clear implications for those formulating these product types.
Presentation
The time course for developing dermatitis varies from hours to days following the dye exposure. Dermatitis symptoms commonly include itching, burning and a rash localizing to the face or scalp margins. It is important to note that the exposed scalp often fails to demonstrate visible inflammation.3 The presentation and dermatitis severity ranges from redness, subtle swelling and irritation of the eyes to intense swelling of the face with exudation of the scalp.
Modern hair dyes color hair convincingly, and colored hair is seldom discernible from natural hair. Thus, a detailed medical history is necessary to determine if the patient is using hair dye when presenting with these symptoms.
Patch Testing
For many years, PPD has been the primary focus in patch test screening for hair dye contact allergy, as it is a known ingredient in hair dye and an extreme sensitizer.2 The frequency of PPD allergy in the general adult population is approximately 1–3%, and salon or self-testing for contact sensitization with PPD formulations is available to identify individuals likely to react upon subsequent hair dyeing.4 A patch test kita can provide an alert of a potential adverse reaction prior to the use of a hair dye.4 Backsetter et al. demonstrated that 90% of those who were moderately to strongly allergic to PPD, according to previous patch testing, were also positive to the patch test kit.
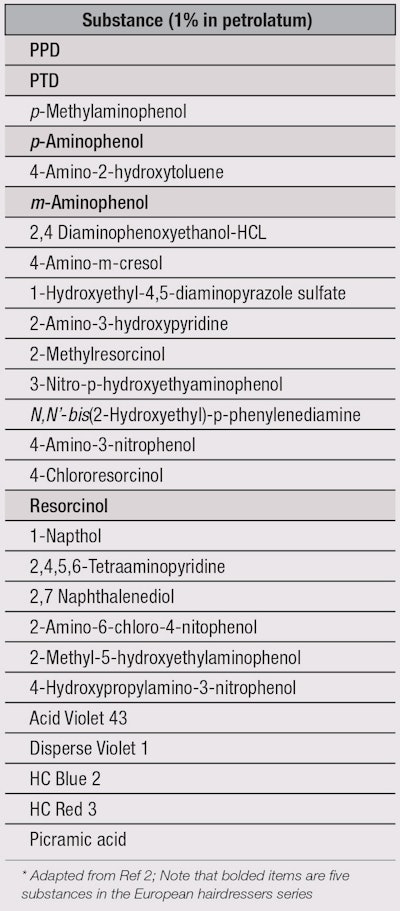
There are approximately 100 other chemicals permitted for use in hair dye, many of which may be clinically important sensitizers not routinely patch tested in patients.5, 6 Sosted et al. performed a quantitative analysis to predict sensitization potential for hair dye chemicals, and discovered 22 potentially allergenic hair dye chemicals in addition to the five chemicals previously identified by the European hairdressers series;2 these are listed in Table 1. While there may be limitations in this study due to the relatively small sample size and low concentrations used, this list remains relevant for identifying the specific agent causing allergic dermatitis. Therefore, it is recommended to have a health care worker complete a patch test for PPD, key chemicals in Table 1 and the ingredients of the particular hair dye in question.
Interventions
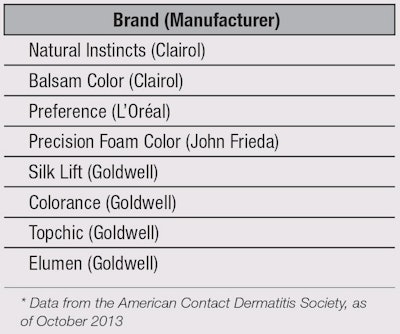
Since PPD is the most common allergen in hair dyes, choosing a synthetic formulation that excludes this ingredient may help allergic individuals to avoid dermatitis.7 In addition, semi-permanent dyes are more likely to be tolerated than permanent dyes due to the lower allergen concentrations used. Herbal and plant products have also been demonstrated to be less allergenic, but may include additives such as diaminotoluenes and diaminobenzenes that can cause contact dermatitis.8 Herbal products and PPD-free products are shown in Table 2.9 Interestingly, Procter & Gamble recently commercialized the PPD derivative 2-methoxymethyl-p-phenylenediamine; this hair dye molecule is believed to have reduced sensitization properties.10
Prevention Principles
If non-allergenic hair dyes are not options, there are application techniques that minimize dye exposure. A common area of skin affected by dermatitis is the scalp margin. A well-trained and experienced hairdresser with good technique can minimize lateral spread of the dye onto the scalp by applying a barrier of petrolatum.11 The least amount of dye possible should be carefully applied to hair, lessening skin and scalp contact. The dye should also remain for the minimum time required to obtain the desired result. Further, it is prudent for consumers to schedule appointments early in the work week, in the event that dermatitis occurs. Most reactions develop within days of exposure to hair dye, so an early appointment affords time to see a health care worker if necessary.
Conclusion
Many consumers with a history of contact dermatitis have previously been advised to avoid hair dyeing. However, with due diligence, understanding individual sensitivities and appropriate preparation, and minimal dye exposure, these consumers are often able to color their hair without complications.
The likelihood of developing allergic contact dermatitis due to hair dye is related to the intensity of the patch test reaction.12 However, it is important to note the hair dye may not contain the necessary concentration for negative exposure during routine use, even if the allergen concentration during patch testing reaches a patient’s biological threshold for reaction.13 Even those with a 3+ positive patch test response are often able to hair dye without resultant dermatitis. One possible explanation relates to the difference between single exposure in dyeing versus multiple exposures. In use testing, i.e., provocative use tests and repeat open application tests, clinical dermatitis occurs with repeated applications as long as three to four weeks later. Generally, the stronger the patch test response, the sooner the use test reaction will occur.13This suggests that many patients can continue to color their hair with proper counseling and informed consent.
References
- JP Thyssen and JM White, Epidemiological data on consumer allergy to p-phenylenediamine, Contact Dermatitis 59 327-343 (2008)
- H Søsted et al, Contact allergy to common ingredients in hair dyes, Contact Dermatitis 69 32–39 (2013)
- H Zhai et al, Reactions of non-immunologic contact urticaria on scalp, face and back, Skin Res Technol 18(4) 436-41 (2011)
- DA Basketter and J English, Pre-testing in hair dye users: An assessment of the Colourstart system, Eur J Dermatol 19 232–237 (2009)
- European Commission, Scientific Committee on Consumer Products, Opinion on p-phenylenediamine (2006)
- European Commission, Scientific Committee on Consumer Products, Opinion on toluene-2,5-diamine (Oct 2, 2007)
- A Scheman, C Cha and M Bhinder, Alternative hair-dye products for persons allergic to para-phenylenediamine, Dermatitis 22(4) 189-92 (2011)
- M Polat, M Dikilitas¸, P Öztas¸ and N Alli, Allergic contact dermatitis to pure henna, Dermatology Online Journal 15(1) (2009)
- American Contact Dermatitis Society, Contact Allergy Management Program Database, available at www.contactderm.org (Accessed Apr 28, 2013)
- C Goebel et al, Introduction of a methoxymethyl side chain into p-phenylenediamine attenuates its sensitizing potency and reduces the risk of allergy induction, available at: dx.doi.org/10.1016/j.taap.2013.11.016 (2013) (Accessed Apr 28, 2013)
- J Ashworth, WS Watson, and AY Finlay, The lateral spread of clobetasol 17-propionate in the stratum corneum in vivo, Br J Dermatol 119(3) 351-8 (1988)
- JP McFadden, L Yeo and JL White, Clinical and experimental aspects of allergic contact dermatitis to para-phenylenediamine, Clinical Dermatology 29(3) 316-24 (2011)
- D Zaghi and HI Maibach, Quantitative relationships between patch test reactivity and use test reactivity: An overview, CutanOcul Toxicol 27(3) 241-8 (2008)