The “Vitamin D Revolution,” as proclaimed by many doctors and experts, is just beginning to uncover the significance of vitamin D for health. In the last decade, vitamin D has gone from recognition primarily for its role in bone health to being investigated for possible roles in a wide range of body functions and in the prevention of diseases—from cancer and diabetes, to multiple sclerosis and depression.
Vitamin D is the only vitamin that the body actually makes. It is made in the skin and converted to a hormone. When vitamin D hormone levels are balanced, auto-immune skin conditions such as eczema, psoriasis and rosacea improve.
As a skin care formulator, this author began three years ago to research vitamin D. Speaking with researchers and medical specialists expanded her appreciation for the critical importance of enhancing vitamin D health inside and outside. Supporting this statement, Michael F. Holick, PhD, MD, wrote in his work, The Vitamin D Solution, “If I had to give you a single secret ingredient that could apply to the prevention—and treatment, in many cases—of heart disease, common cancers, stroke, infectious diseases from influenza to tuberculosis, dementia, depression, insomnia, joint pain, rheumatoid arthritis, osteoporosis, psoriasis and hypertension, it would be this: Vitamin D.”
There are two principle types of vitamin D: D2 and D3, as well as other active analogs. Ergocalciferol (D2) is derived from sources such as fortified milk, herring, mackerel, tuna, salmon, sardines, eggs, fortified cereals and baked goods. Vitamin D3, otherwise known as cholecalciferol, is photochemically produced upon UV exposure from the precursor sterol 7-dehydrocholesterol, which is present in the epidermis. Vitamin D3 is an essential nutrient and pro-hormone; it, too, is present in animal products and fortified foods, and can be consumed from fish oil, eggs or fish. This article describes a pilot study researching the potential for topical vitamin D3 delivery.
Vitamin D History and Deficiency
The first scientific description of a vitamin D deficiency, namely rickets, was provided in the 17th century by both Whistler1 and Glisson. Then in 1861, Trousseau associated rickets with a lack of sunlight exposure. However, years passed before the work of Mellanby and McCollum in 1918, which led to the discovery of vitamin D.1
As noted, vitamin D production begins as a chemical reaction in the skin upon exposure to UV light—specifically UVB. With age, skin loses its ability to produce sufficient levels of vitamin D. The skin needs vitamin D to make vitamin D; therefore depletion in the skin also limits its production. Besides aging, vitamin D deficiency can occur due to inadequate exposure to the sun, skin color, geography or low levels in the diet. As the body draws on vitamin D to make more, it destroys the vitamin D used in the creation process. This cycle therefore requires more to be constantly replenished.
To reach optimal levels, it should be produced in the skin as well as supplied through a diet rich in vitamin D. At present, vitamin D supplements are available as oral and injection forms; however, compliance of oral vitamin D supplementation alone is only reported to be 20-60%.Therefore, another reason the author was interested in supplementation of vitamin D by a topical route was to increase patient compliance. Estimates show that one billion people worldwide, a figure that grows in winter months, are vitamin D deficient.2 Seventy-six percent of pregnant women are severely vitamin D deficient, and nearly half (48%) of girls ages 9-11, a sizable percentage being minorities or individuals of darker skin, e.g., Hispanic, Black and Asian, also are deficient in vitamin D.3 It is interesting to note that in the 1980s, the Saudi population showed low vitamin D levels; extensive work by Sedrani et al. further revealed this deficiency existed not only during winter months, but also summer months due to non-exposure to the sun. Al-Turki et al. and Sadat-Ali et al. additionally found that, in the healthy Saudi population, vitamin D deficiency occurred in approximately 40-60% of men and women over the age of 50.
Delivery of Vitamin D3
Research suggests that supplemental vitamin D could block the inflammatory process of psoriasis, and that synthetic vitamin D delivered topically via prescription ointments is effective in treating psoriasis.4 Additionally, the use of UV light therapy in conjunction with vitamin D creams has been found effective. Jurgen Schauber, MD, of Ludwig-Maximillian University in Germany, explained that along with other proteins, vitamin D is a key player in activating an inflammation-triggering inflammasome, which helps autoimmune skin conditions. Topical vitamin D treatments and UVB light therapy help DNA to inhibit inflammasome activation by controlling cathelicidin production. In relation, Henry Lim, MD, chief of dermatology at the Henry Ford Hospital in Detroit, noted this study increases the understanding of the role of vitamin D in psoriasis.
“We have used these treatments for a long time, but we haven’t had a full understanding of why they work,” Lim said, in a report by WebMD. “This is one potential mechanism.”5
Recent studies also show that natural forms of vitamin D—D3 in particular—can be safely delivered by topical skin creams. This latter work inspired studies in Dubai to determine whether the topical application of vitamin D could not only enhance the external skin condition, but also elevate its internal production.
Case Study: Vitamin D in the Bloodstream
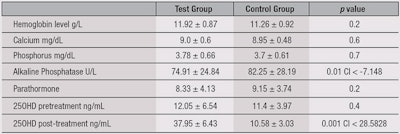
To test the topical delivery of vitamin D, a randomized, controlled study was conducted in 2014 at the College of Medicine, University of Dammam, King Fahd Hospital of the University, AlKhobar, in Saudi Arabia.6 The purpose of the study was to determine the feasibility of topically applied vitamin D to transdermally enhance levels of vitamin D in the bloodstream. Forty-eight healthy female medical students participated in the research. Following medical history and clinical exams, their blood was initially drawn for 25 Hydroxy Vitamin D3 (25OHD) levels, which were measured by chemiluminescence immunoassay (CLIA). In the United States, 30 mL is threshold to describe vitamin D sufficiency; thus > 30 mL was taken as normal, 21-29 mL as insufficient and < 20 mL as deficient.
The participants were then divided into two groups of 24 each. They agreed not to change their dietary habits or lifestyles, including sun exposure, until three months later—after the study ended. The first group applied topical vitamin D3 using an aloe vera-based cream, with each gram of the cream delivering 5000 IU of vitamin D3. The second group used 1 g of aloe vera gel without vitamin D. The participants had no knowledge to which group they belonged. A second blood sample was taken after three months, and the data was analyzed.
In the control group, no statistically significant change in 25OHD levels was observed (see Figure 1). In fact, the average was slightly lower than the initial results at the onset of the study. In the test group, women who had initial lower levels of 25OHD showed marked improvements. The average 25OHD in the test group pre-treatment was 12.05 mL ± 6.54, and post-treatment was 37.95 mL ± 6.43 (p ≤ 0.0001). In the control group (see Figure 2), the pre-treatment 25OHD was 10.4 mL ± 3.97 and post-treatment was 9.58 mL ± 3.03. The comparison between the two groups is shown in Table 1.
This study shows that vitamin D3 could effectively be delivered by dermal route, reducing the incidence of non-compliance of oral route; furthermore, no incidents of rashes or reactions were observed with topical treatment. While the most common routes of administering vitamin D are oral or invasive/injectable, the present findings suggest a third route: transdermal. For any drug, large proportions of oral prescriptions are never taken at all.7 Recent estimates for noncompliance range from study to study, with 62% to 84% using electronic monitoring.8, 9 Hence, these authors believe that in the young and elderly, the oral route can be bypassed by the use of transdermal route. Note that the described study was funded and conducted by the University of Dubai. However, the author’s company used this study data, along with other ongoing studies, to develop product concepts for a topical vitamin D.
Since there is little research to indicate that supplements can actually make their way past the acidic internal process and be deposited in skin,10 topical application of antioxidants and minerals has become a focal point among the medical community. This, taken in conjuction with the described results, led to the development of a concept combining nutritional and topical approaches to deliver ingredients, such as vitamin D; in this case, a whole food spice powdera and topical elixir skin care lotionb was created for an inside-out approach.
Conclusions
Application of topical products to the skin can act locally, pass into the systemic circulation, or do both. Although the stratum corneum (SC) is an efficient barrier, some substances are able to penetrate it to reach the underlying tissues and blood vessels. These substances must be lipophilic, and since vitamin D is fat-soluble, it should be able to cross the skin barrier. To assist in their delivery, however, penetration enhancers may be employed. The most ideal penetration enhancer discovered to date is water; hydrating the SC has been shown to increase the penetration of both hydrophilic and hydrophobic drugs.
The present study also shows that with a daily dose of topical vitamin D, within a 90-day period, 25OHD blood levels returned to a minimum normal level of 30 mL. In conclusion, the results of this study indicate that topical vitamin D penetration is possible, efficacious and safe for the young as well as the elderly. Additional studies are being conducted to establish the cosmetic benefits of topical vitamin D to enhance skin conditions in participants who saw elevated vitamin D levels in the bloodstream.
References
- www.gpcme.co.nz/pdf/GP%20CME/Friday/C1%201425%20Harrison.pdf (Accessed Apr 1, 2015)
- www.ncbi.nlm.nih.gov/pubmed/18400738 (Accessed Apr 1, 2015)
- www.naturalnews.com/003069.html (Accessed Apr 1, 2015)
- MK Batra and J Ropp, Improved cosmetic effect of topical cream containing vitamin D2 and D3, San Diego, CA (Jul 2012)
- Y Dombrowski, News release, Science Translational Medicine vol 3 (May 11, 2011)
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3976443/ (Accessed Apr 1, 2015)
- J Avorn, Medications and the elderly, in J Rowe and R Besdine, eds, Geriatric Medicine, 2nd edn, Little, Brown, Boston (1988)
- P Koch-Gwinner et al, Measurement of drug compliance by continuous electronic monitoring: A pilot study in elderly patients discharged from hospital, J Amer Geriatrics Soc 40 1151–1155, 11 (1942)
- T Nikolaus et al, Elderly patients’ problems with medication. An in-hospital and follow-up study, Eur J Clin Pharmacol 49(4) 255–259 (1996)
- Viruses and Diseases, Harvard Health Publications, in collaboration with MN Starnbach, Harvard Medical School (2013)