Substances known to impart a sensation of warmth upon application are called warming agents and include capsicum (red pepper), ginger extract and vanillyl alcohol alkyl ether derivatives. Capsicum is the material used most as a warming agent in personal care; however, its side effects may include skin irritation, burning, itching and possible carcinogenicity.1 In relation, vanillyl alcohol alkyl ether derivatives, specifically vanillyl butyl ether (VBE), was investigated as an alternative, milder warming agent for personal care applications.
Vanilloids contain vanillyl groups that bind to the transient receptor potential type V1 channel (Vanilloid receptor-1, TRPV1), a nonselective cation channel that naturally responds to noxious stimuli such as high temperatures and acidic pH.2, 3 This binding of the vanilloid to TRPV1 opens the channel pore, which leads to an influx of predominantly calcium cations.4 In turn, this action causes membrane depolarization that, once reaching a threshold level, generates an action potential that is propagated along the axon to the synapse.5 Activated neurons will release glutamate, adenosine triphosphate (ATP) and a variety of neuropeptides as transmitters from the synapse. These neurotransmitters launch a cascade and eventually reach the central nervous system.2
According to a previous study, capsicum similarly causes a warming sensation through the central nervous system and vasodilation delivery to vascular endothelial cells.2, 3, 6 While evidence has indicated that vasodilation can be examined using laser Doppler flowmetry,5, 7–9 the present study shows how measurements of local blood cell flux (BCF) taken via laser speckle contrast imaging provide results that are unaffected by adjacent treatment zones. This method is used here to assess the warming effects of VBE applied in various concentrations in topical creams (see Formula 1).
Materials and Methods
Twenty-one volunteers including 14 females and 7 males, 21–40 years old, having healthy and non-allergic skin (self-assessed) were recruited for the present study. Volunteers washed their forearms with a mild neutral detergent formulated for skin, after which they rested for 20–30 min in an air-conditioned room under constant temperature (22 ± 1°C) and humidity (40–65%). Their relaxation was maintained throughout the procedure and monitored using laser speckle contrast imaging at the untreated site.
Prior to application of the test formulation, the BCF of the test sites was also monitored using a laser speckle contrast imagera until it stabilized, then recorded for 5 min. Four different 0.01-g sample creams including various percentages of VBE, i.e. 0%, 0.1%, 0.3% and 0.5%, were applied to each subject’s forearm within the 1.5 x 1.5-cm2 labeled area. An untreated site was monitored for the relaxed state, and each site served as its own control in the first 5 min. The VBE-induced increase in BCF after application was assessed for 45 min continuously using the laser imagera; results were analyzed using specialized softwareb.
Results
From the blood flow curve diagram of volunteer 14, which was the most representative of the whole, it can be seen that the perfusion remained constant during the first 5 min before application in all treated sites (fluxes 2–5), and during the period of monitoring the untreated site (flux 1) (see Figure 1). After application, the 0.1%, 0.3% and 0.5% VBE creams showed an increase in BCF as denoted by the changes in the blood flow curve. For the untreated and 0% VBE cream zone, no significant increase in perfusion was shown in this particular individual.
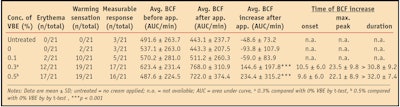
From the blood flow images of volunteer 14 (Figure 2), it was apparent that the application of VBE cream increased BCF. The sites treated with 0.3% and 0.5% VBE cream show a distinct increase in BCF. The response of a warming sensation and the average BCF were shown to increase 45 min after application; the results for all 21 subjects are summarized in Table 1.
Seventeen of the 21 volunteers (80.95%) showed an increase in perfusion with the 0.3% VBE cream; 16 volunteers (76.19%) showed an increase with the 0.5% VBE cream; and five volunteers (23.81%) showed an increase with the 0.1% VBE cream. Dose-related increases in erythema, warming sensation and BCF were observed after application of the VBE cream.
This warming sensation was further evaluated by self-assessments from the volunteers. Two subjects reported a warming sensation at the 0% VBE cream site, which could be caused by confusion of the sensation from the adjacent site of VBE cream application. Ten volunteers felt a warming sensation with the 0.1% VBE cream, and a total of 19 volunteers felt warmth after application of both 0.3% and 0.5% cream.
In addition, a phenomenon was observed immediately after application of the cream: the average perfusion in all treated sites decreased because the perfusion of the 0% and the 0.1% VBE cream site did not return to baseline, which led to a negative value in the average perfusion increase after application. The average BCF value increased after application of 0.3% and 0.5% VBE cream, 144.6 ± 197.8 (p < 0.001) and 234.4 ± 315.2 (p < 0.001), respectively (see Table 1).
The percent increase in BCF was significant in both 0.3% and 0.5% VBE cream-treated sites. The 0.3% VBE cream showed a 24.22% (p < 0.001) BCF increase, and the 0.5% VBE cream showed a 54.74% (p < 0.001) BCF increase (see Figure 3). The onset time of perfusion increase and the peak response time were related to the dosage of VBE in the cream formulation in all the measurable respond volunteers.
Subjects also reported the onset and maximum peak warming sensation occurred faster with the 0.5% VBE cream than the 0.3% VBE cream, and the average duration of the perfusion in all 21 individuals was more than 30 min. Neither erythema nor a warming sensation was observed in response to the untreated zones, and no subject experienced pain or discomfort at the treatment sites. There were individual variations among the volunteers but mean perfusion, warming sensation and erythema were dose-dependent.
Formulating with VBE
The warming mechanism of VBE is activated only when its functional group, the vanillyl group, interacts with the vanillyl receptor on the skin. The solubility of VBE with other ingredients is a key factor that would affect the releasing level of VBE from the formulation to impart a warming sensation. VBE is oil-soluble and it is more stable in emulsions than in water solutions, thus it is recommended that the phase inversion temperature (PIT) method be used when adding VBE in formulations, to encapsulate VBE in the emulsion.
When formulating a PIT emulsion, the oil phase and part of the water in the formulation must be heated to above the PIT temperature. Initially, a w/o phase formulation is formed when the heated water is slowly added to the oil phase. As the emulsion cools, oil particles will be packed by water molecules, forming the final o/w phase formulation. VBE should be added into the formulation as the temperature approaches PIT and not after the phase inversion.
Conclusions
Here, laser speckle contrast imaging was successfully used to investigate the effects of 0.1%, 0.3% and 0.5% VBE in topical formulations on local BCF. The authors propose that after immediate application of the creams, differences in temperature between the test formulations on the skin of the volunteers, approximately 37°C, may have evoked constriction in the vessels, thus resulting in lowered BCF. After a short time, the BCF increased, which is an effect of the VBE acting on vasodilation. However, some individuals showed a warming sensation without a measurable increment in BCF. As described, results indicate that the warming sensation imparted by VBE has a direct correlation with its concentration.
The duration of BCF increase lasted more than 30 min, and the BCF did not return to its original level. This, in part, is likely due to the fact that the experiment was monitored for only 45 min after application; in the future, the test could be evaluated for greater than 45 min to observe the BCF return. The described experiments can be conducted further with different arms or fingertips to examine the increase in blood cell flux by VBE.
While individual variations in results existed among the volunteers, it is proposed that physiological and other factors such as basal BCF, body temperature and movement during the testing process could have impacted the results. A larger sample size with different ages and genders will be considered in a future investigation.
References
Send e-mail to [email protected], or to [email protected].
- MK Hwang, AM Bode, S Byun, NR Song, HJ Lee, KW Lee and Z Dong, Cocarcinogenic Effect of Capsaicin Involves Activation of EGFR Signaling but Not TRPV1, Cancer Research 70 (17): 6859–6869 (2010)
- A Szallasi and PM Blumberg, Vanilloid (capsaicin) receptors and mechanisms, Pharmacol Rev 51(2) 159–212 (1999)
- D Julius and AI Basbaum, Molecular mechanisms of nociception, Nature 413 203–210 (2001)
- JN Wood, J Winter, IF James, HP Rang, J Yeats and S Bevan, Capsaicin-induced ion fluxes in dorsal root ganglion cells in culture, J of Neuroscience 8 3208–3220 (1988)
- P Holzer, Capsaicin: Cellular targets, mechanisms of action and selectivity for thin sensory neurons, Pharmacol Rev 43 143–201 (1991)
- T Kark et al, Tissue-specific regulation of microvascular diameter: Opposite functional roles of neuronal and smooth muscle located vanilloid receptor-1, Mol Pharmacol 73(5) 1405–1412 (2008)
- R Crompton, VL Clifton, AT Bisits, MA Read, R Smith and IMR Wright, Corticotropin- releasing hormone causes vasodilation in human skin via mast cell-dependent pathways, J of Clin Endocrin and Metabol 88(11) 54
- TA Munce and WL Kenney, Age-specific skin blood flow responses to acute capsaicin, J of Gerontology, 58A (4) 304–310 (2003)
- BJ Van der Schueren et al, Reproducibility of the capsaicin-induced dermal blood flow response as assessed by laser Doppler perfusion imaging, Brit J of Clinical Pharma 64(5) 580–590 (2007)