The pursuit of hygiene leaves the largest footprint on the skin’s surface, since cleansing procedures are the most oft-performed. From eight to 10 applications of hand soap per day, to bathing and shampooing, proper cleansing practices are essential to keep possible skin problems at bay; or in the case of atopic dermatitis (AD) management, to remove debris, crusts, exudates and microbial agents that can cause skin infection and trigger irritation.
Surely, during the entire cleansing routine, the correct use of products can prevent much of the skin damage often attributed to cleansing. This includes using the right amounts; adequate rubbing force and duration; and care devoted to the rinse-off phase in order to avoid excessive adsorbtion of surfactant residue onto the skin.
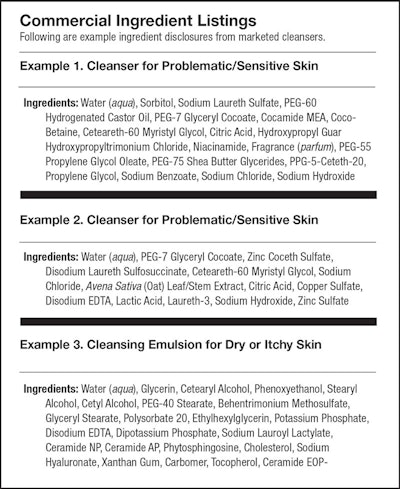
To create the “right” cleanser, one must question: Are there ingredients that must absolutely be omitted from formulas? Or, is it more that the complex of ingredients as a whole requires proper balancing? Depending on the product goals and condition of the targeted skin, it will be important to consider which formulation strategy will provide the “ideally correct” blend.
Compromised Skin
Skin disease is among the leading causes of global disease burden, affecting millions of people worldwide.1 Aging, trauma and environmental and genetic factors can result in the onset of several skin diseases, with more than 3000 entities identified in literature.2, 3
Some facts and figures on AD and other skin diseases include:
- The prevalence of AD is estimated to be 15-20% in children and 1-3% in adults; additionally, its incidence has increased by two- to threefold in industrialized countries during recent decades.
- The International Study of Asthma and Allergies in Childhood (ISAAC) can provide some of the most valuable prevalence and trend data concerning AD; it covers close to 2 million children in 100 countries, and is the largest and only allergy study to have taken a truly global approach.4
- Nearly 85 million Americans (27% of the population, or more than one in four individuals) complained of a skin disease and were seen by a physician in 2013.5
- In most industrially advanced markets, acne is generally thought to be the most common dermatosis, affecting approximately 85% of the population at some point in life.6
Moreover, eczema is a common dermatologic condition characterized by erythema, desquamation, papulation, lichenification, excoriation and itching. It affects children as well as adults, both males and females, and is related to a defective skin barrier, most commonly due to damage to the intercellular lipids caused by the improper selection of skin cleansers and moisturizers.
Hygiene procedures are frequent during the day and as stated, the overuse of cleansers can lead to epidermal barrier damage, increasing transepidermal water loss. This, in turn, has been associated with itch intensity in patients affected by eczema.7
Surfactants and Skin
Surfactants, in particular, are the major ingredients of body soaps and cleansers, and harsh varieties have been suggested to damage the skin. Thus, while the stratum corneum (SC) is rich in intercellular lipids, its structure can be easily disrupted by surfactants, consequently impairing barrier function of the skin.
Numerous studies and reviews describing the interaction between surfactants and the skin8-11 have sought to link the physicochemical properties of surfactants to their toxicity. Such studies have mainly been performed using ionic surfactants, generally known to be more irritating than nonionic surfactants.12-14 Indeed, ambiguity still exists over which physical characteristics of a surfactant system are the most important for obtaining mildness and fair skin compatibility.
Publications detailing the effects of surfactants on membrane permeability describe an apparent concentration-dependent biphasic action. An increase in membrane permeability occurs at low surfactant concentrations but this decreases at higher concentrations, generally above the critical micelle concentration (CMC) of the surfactant.15
Micelles were discovered to be capable of penetrating the SC; therefore, both monomeric and micellar surfactant species should be considered.16, 17 The presence of surfactant micelles in solution is necessary for the solubilization of lipid material and, in comparison with other assembled structures, e.g., cylinder, lamels, etc., spherical micellar solutions usually solubilize a small amount of fatty materials. The micelle size and surface charge18 are also important physical characteristics, as they influence the micelle stability and their power to affect skin lipids.
The pursuit of hygiene leaves the largest footprint on the skin’s surface.
The amounts of solubilized lipids are dependent upon:
a) the individual strengths of hydrophilicity and lipophilicity of the amphiphile. Surfactants having the same HLB can solubilize larger amount of lipids when they have longer alkyl chains; and
b) size. The micelle size increases with the increase in the alkyl chain length, even with the same HLB.19
We could simplify these interactions to three possible profiles of membrane alteration induced by surfactants, as a function of surfactant concentration (see Figure 1). Profiles A and B represent the situation where alteration is increased at premicellar concentrations. The formation of micelles decreases or maintains the capability of the surfactant to penetrate the SC. Profile C represents the case where the surfactant increases its ability to affect the integrity of the skin membrane, both before the micelle formation and after reaching its CMC.
In practice, between the mid-1980s and early 1990s, scientists realized the proper combination of different surfactants can significantly reduce protein damage and skin and irritation due to cleansing. As an example, adding amphoteric surfactants at about 20-30% of the concentration of an accompanying anionic surfactant will reduce the charge density, and thereby stabilize micelles of anionic surfactants. According the micelle theory, as mixed micelles are less likely to break apart, less surfactant monomer is able to enter the SC and damage lipids and proteins. On the other side, it should be noted that the equilibrium of micelles-monomers requires less than a few seconds to occur; in other words, it is not just the micelle or monomer state that strictly determines skin aggressivity. The most promising combinations of surfactants adopt balanced blends of the three categories: i.e., anionics, amphoterics and nonionics (see Formula 1).
One additional factor to consider is that some surfactants (i.e., anionics) are harsh toward skin proteins such as keratin, while others (i.e., nonionics and amphoterics) are aggressive toward lipid materials. Balanced surfactant combinations seem to be the best formulation strategy in respect to the overall skin barrier.
Indeed, the addition of C16 and C18 fatty acids to a sodium cocoyl isethionate-based bodywash was found to reduce both protein and lipid damage. The fatty-acid-containing bodywash also reduced skin dryness and TEWL in human volunteers.20 In relation, more recently, the reputed mildness of nonionic surfactants was discussed, highlighting that the difference in charge between the polar head group and lipophilic chain is not the only parameter to be considered.21
Today, formulations are often developed with surfactants that are partially derived from renewable sources—these include plant oils chemically modified with an added polar group to create “natural surfactants.” It is important to note that these surfactants are not inherently milder and suffer the same trade-offs between mildness and performance as other surfactants.22