Depending on a drug or cosmetic ingredient’s intended target, topical delivery systems are broadly categorized as either transdermal drug or dermal drug/cosmetic.1 Transdermal drug delivery (TDD) is the controlled release of drugs through intact skin to obtain therapeutic levels systematically and to affect specified targets for specific purposes such as contraception, among others. Dermal drug/active cosmetic ingredient delivery (DDD) is similar to TDD except that the specified target is the skin itself.1,2 Cosmetic ingredients, including those for antiaging, known as cosmeceuticals, presumably may have the same site of action. The cosmetic and/or transdermal route is indeed desirable by the industry but the success of DDD and cosmetic active ingredient delivery (CAID) technologies remains limited and faces many challenges, one of which is low skin permeability that hinders the development of DDD/CAID for macromolecules.
Overcoming the skin barrier safely and reversibly while enabling percutaneous absorption is a fundamental problem in the field of CAID, TDD and DDD. Advances have been made in recent decades to overcome skin barrier properties,3,4 including physical means such as iontophoresis, sonophoresis and microneedles; chemical means using penetration enhancers; and biochemical means such as liposomal vesicles and enzyme inhibition. A rich library of textbook literature summarizes these extensive experimental backgrounds—largely within the last half of the 20th century.5,6
CAID Systems
CAID systems are capable of delivering localized effects while minimizing systemic side effects and they are the primary modalities for dermatologic treatment or cosmetic purposes. Examples include topical antiaging products, photo-protective materials, cosmetics and moisturizers. Many cosmetic formulations use chemical penetration enhancers to overcome the skin barrier. Again, percutaneous absorption remains a key issue to the success of CAID technology.
As a model for CAID, delivery systems of topical corticosteroids and their pharmacokinetic/pharmacodynamic relationships have been studied extensively as aids to optimizing topical treatment.7-9 For instance, the correlation between the bioavailability of topical corticoids and the thermodynamic activity of the medicament in different bases have been studied.10, 11 Unfortunately few such in vivo human studies have been performed for active cosmetic ingredients.
In a similar investigation, Leopold and Maibach12 characterized local anesthetics pharmacodynamically by measuring thermal thresholds over time with a thermal sensory analyzer (TSA) in human subjects. The results showed that the local anesthetics investigated affect thermal thresholds to a different extent, and that linear relationships exist between cold sensation parameters and the solubility of the local anesthetic bases in medium chain triglycerides and with the drug flux at 50% saturation.
Such examples—i.e., correlation of physical chemistry, percutaneous penetration and pharmacodynamic relationships—are relatively limited and the authors believe that greater exploration in this area will eventually enhance the efficacy of active cosmetic ingredients and consumer satisfaction.
Clinical Relevance of In Vitro Data
The methods employed for studying percutaneous absorption range from in vivo systems, in which the full range of physiological processes are operative, to simple in vitro methods and modeling approaches. Percutaneous absorption can be studied with in vitro methods since it is possible to maintain the barrier properties of the stratum corneum (SC) in excised skin.
There are advantages of using in vitro methods, not in the least that human skin can be used and that procedures are not conducted with animals. Disadvantages include the lack of provision of pharmacokinetic data, and the difficulty of obtaining human skin in sufficient quantities. Attempts have been made to produce simple models of these processes, which have resulted in the development of several of in vitro systems.13-15 An appreciation of the limitations of such processes has enabled the application of the data generated by in vitro methods to be applied with increasing confidence for predicting the likely effects of chemicals in vivo.
Wester and Maibach16 compared in vitro and in vivo methods studying percutaneous absorption and suggested that there were notable differences such that in vitro methods alone would not always be a reliable or accurate predictor of percutaneous absorption in living humans. On the other hand, there is also some evidence that in vitro data can be predictive for in vivo percutaneous absorption in both animals and humans.17,18
However, the current database is limited and the variance often exceeds 1log. In short, only human skin should be used to provide data for risk assessment purposes or for the prediction of therapeutic effects, because there are major differences in the skin permeability properties of animal and human skin17,19 and the use of animal skin often results in an over-prediction of likely human percutaneous absorption.
Presently there are no internationally approved guidelines to conduct in vitro tests to measure percutaneous absorption. Draft guidelines for in vivo and in vitro percutaneous absorption studies have been proposed by the Organization for Economic Cooperation and Development (OECD).20 Discussion documents also have been produced by the US Environmental Protection Agency (EPA) and the US Food and Drug Administration (FDA), prompting much discussion for the principles of conducting percutaneous absorption measurements.14,21 In spite of several national and international standardization efforts by the EPA, the European Centre for the Validation of Alternative Methods (ECVAM) and the OECD,14 the industry still lacks a complete in vivo validation method that is relevant in humans.
Percutaneous Enhancers for Cosmetic Actives: An Overview
The difficulty in validating clinically relevant in vitro percutaneous absorption systems lies in the complexity of percutaneous penetration. Wester and Maibach16 proposed that the process of percutaneous absorption can be examined through ten steps. These steps start with vehicle release of chemical to the skin and proceed into the various kinetics and factors affecting percutaneous absorption (see Ten Steps to Percutaneous Absorption).
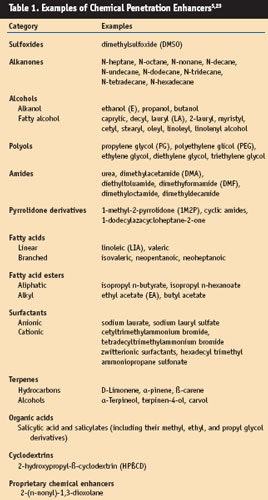
Given the many complex aspects of percutaneous absorption, with the greatest hindrance to it being the SC, extensive research has been conducted and innovations designed in the field of penetration enhancement. The literature is abundant with articles, patents and reviews on this topic.5 In the sidebar, Common Penetration Enhancement Techniques, and Table 1, common penetration enhancement techniques and examples of chemical penetration enhancers are listed.
Yet despite the plethora of candidate penetration enhancement techniques, few have enjoyed wide scale medical acceptance. Hydration by occlusive systems or topical vehicles remains the most facile way to obtain a reduction in barrier potential of the SC. To date, clinicians, cosmetic chemists and pharmaceutical scientists still regard chemical induced occlusion as a convenient and safe method of enhancing CAID.22
Conclusion
Taken together, extensive experimentation has led to some medical acceptance of methods of enhancing flux, such as the solubilization of active cosmetic ingredients with propylene glycol. However, much remains to be achieved and there is little data available on the penetration of cosmetic actives.
In the authors’ view, more and rapid progress will occur with experienced multidisciplinary teams consisting of cosmetic and pharmaceutical chemists, physical chemists, engineers, dermatotoxicologists, dermatologists, etc.—leading to more effective and safe active cosmetic ingredients.
Reproduction of all or part of this article strictly is prohibited.
References
Send e-mail to [email protected]
1. AF Kydonieus, JJ Wille and GF Murphy, Fundamental concepts in transdermal delivery of drugs, Biochemical Modulation of Skin Reactions: Transdermals, Topicals, Cosmetics, AF Kydonieus and JJ Wille eds., CRC Press: Boca Raton, FL, 1–14 (2000)
2. MB Brown, GP Martin, SA Jones and FK Akomeah, Dermal and transdermal drug delivery systems: Current and future prospects, Drug Deliv 13(3) 175–187 (2006)
3. BW Barry, Penetration enhancer classification, Percutaneous Penetration Enhancers, 2nd Edition, EW Smith and HI Maibach eds., CRC Press: Boca Raton, FL, 3-16 (2005)
4. A Nanda, S Nanda and NM Ghilzai, Current developments using emerging transdermal technologies in physical enhancement methods, Curr Drug Deliv 3(3) 233–242 (2006)
5. EW Smith and HI Maibach eds., Percutaneous Penetration Enhancers, 2nd Edition, CRC Press: Boca Raton, FL (2005)
6. RL Bronaugh and HI Maibach eds., Percutaneous Absorption: Drugs, Cosmetics, Mechanisms, Methods, 4th Edition, Taylor & Francis: Boca Raton, FL (2005)
7. BW Barry, Bioavailability of topical steroids, Dermatologica 152 supp1 47–65 (1976)
8. MK Polano, M Ponec, G Smeenk, and JC Hendrikse, Factors influencing the penetration of corticosteroids through the epidermis, Adv Biol Skin 12 325–338 (1972)
9. BM Magnusson, SE Cross, G Winckle and MS Roberts, Percutaneous absorption of steroids: Determination of in vitro permeability and tissue reservoir characteristics in human skin layers, Skin Pharmacol Physiol 19(6) 336–342 (2006)
10. R Woodford and BW Barry, Optimization of bioavailability of topical steroids: Thermodynamic control, J Invest Dermatol 79(6) 388–391 (1982)
11. SL Bennett, BW Barry and R Woodford, Optimization of bioavailability of topical steroids: Non-occluded penetration enhancers under thermodynamic control, J Pharm Pharmacol 37(5) 298–304 (1985)
12. CS Leopold and HI Maibach, Percutaneous penetration of local anesthetic bases: Pharmacodynamic measurements, J Invest Dermatol 113(3) 304–307 (1999)
13. RL Bronaugh, MEK Kraeling and JJ Yourick, Determination of percutaneous absorption by in vitro techniques, Percutaneous Absorption: Drugs, Cosmetics, Mechanisms, Methods, 4th Edition, RL Bronaugh and HI Maibach eds., Taylor & Francis: Boca Raton, FL, 265–270 (2005)
14. D Howes et al, Methods for assessing percutaneous absorption: The report and recommendations of ECVAM workshop, ATLA 24 81–106 (1996)
15. RL Bronaugh and SW Collier, Protocol for in vitro percutaneous absorption studies, In Vitro Percutaneous Absorption: Principles, Fundamentals and Applications, RL Bronaugh and HI Maibach eds., CRC Press: Boca Raton, FL, 237–241 (1991)
16. RC Wester and HI Maibach, Cutaneous Pharmacokinetics: 10 Steps to Percutaneous Absorption, Drug Metab Rev 14 (2)169–205 (1983)
17. RL Bronaugh and HI Maibach, Percutaneous absorption of nitroaromatic compounds: In vivo and in vitro studies in human and monkey skin, J Invest Dermatol 84 180–183 (1985)
18. SA Hotchkiss, MAJ Chidgey, S Rose and J Caldwell, Percutaneous absorption of benzyl acetate through rat skin in vitro. I. Validation of an in vitro model against in vivo data, Food Chem Toxicol 28 443–448 (1990)
19. RC Scott, MW Walker and PH Dugard, A comparison of the in vitro permeability properties of human and some laboratory animal skins, Int J Cosmet Sci 8 189–194 (1987) 2
0. Anon, Proposal for two new guidelines on percutaneous absorption, OECD Environmental Health and Safety Division Discussion Document, ref. ENV/EHS/HK/mc/94.103, OECD, Paris, 1–18 (1994)
21. Anon, Dermal Exposure Assessment: Principles and Application, US Department of Commerce, Environmental Protection Agency Report No. EPA/600/8-91/011B, US Department of Commerce, Washington, DC, 1–450 (1992)
22. J Zhang, CH Purdon, EW Smith, HI Maibach and C Surber, Penetration enhancement by skin hydration, Percutaneous Penetration Enhancers, 2nd Edition, EW Smith and HI Maibach eds., CRC Press, Boca Raton, FL, 67–72 (2005)
23. SC Chattaraj and RB Walker, Penetration enhancer classification, Percutaneous Penetration Enhancers, 1st Edition, EW Smith and HI Maibach, eds., CRC Press: Boca Raton, FL, 5–20 (2005)